Comment:
This one’s a favorite for several reasons. It’s published in JAMA Internal Medicine, which is about as conventional of a journal as you can get.
The authors freely admit that the results of the studies are heterogenous enough that they didn’t satisfy the requirements and really should have not gone ahead with the meta-analysis.
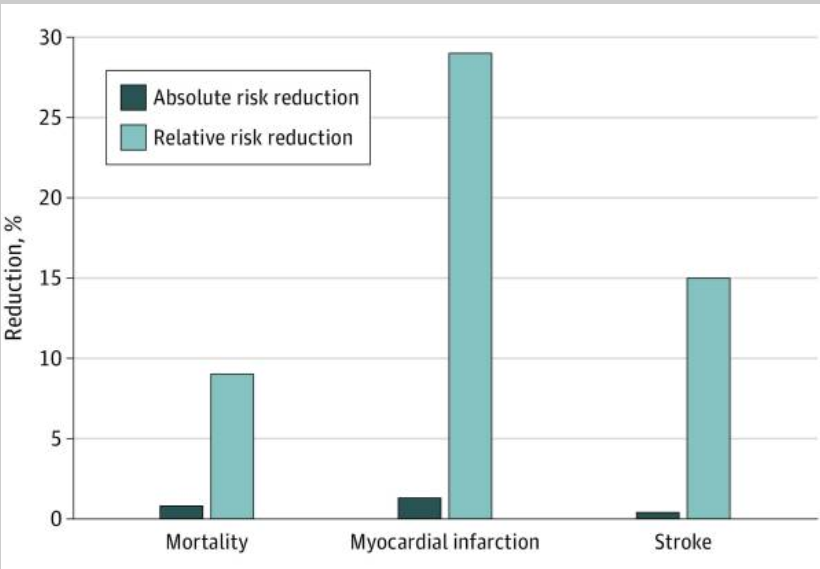
And even with ignoring the high I2 value they could only show reductions in the 1% range: 0.8% mortality, 1.3% for all MIs which includes minor events, and 0.4% for stroke.
Summary:
Clinical Bottom Line
This meta-analysis of 21 randomized trials suggests that while statins are associated with a statistically significant reduction in cardiovascular events when measured in relative terms, the absolute benefits for patients are modest. More importantly, the certainty of this evidence is reduced by significant inconsistency (heterogeneity) across the included trials, and the analysis was unable to establish a conclusive link between the degree of LDL-C reduction and the size of the clinical benefit for mortality, MI, or stroke. Therefore, the true magnitude of benefit from statins is debatable, and these findings underscore the importance of discussing the small absolute risk reductions with patients.
Results
Summary of Results
The meta-analysis pooled results from 21 trials and found the following effects for statin therapy compared to placebo or usual care:
-
All-Cause Mortality: An absolute risk reduction (ARR) of 0.8% and a relative risk reduction (RRR) of 9%.
-
Myocardial Infarction (MI): An ARR of 1.3% and a RRR of 29%.
-
Stroke: An ARR of 0.4% and a RRR of 14%.
The authors note that reporting the 29% relative risk reduction for MI without its corresponding 1.3% absolute risk reduction can be misleading. The small absolute benefit means that 77 participants would need to be treated with a statin for an average of 4.4 years to prevent just one myocardial infarction.
Assertive Critical Appraisal
Certainty of Evidence (GRADE Framework)
The authors used the GRADE framework to assess the certainty of the evidence for each outcome. Due to significant inconsistency across the trials, the certainty of the evidence was downgraded for several key outcomes. For example, the evidence for all-cause mortality across all trials and for all stroke outcomes was rated as “moderate to low certainty.” This formally acknowledges that our confidence in the estimated effect is limited.
Heterogeneity
The analysis found significant statistical heterogeneity, which suggests that the results of the individual trials were inconsistent.
-
Definition: The heterogeneity statistic, I2, represents the percentage of variation across studies that is due to genuine differences in effect rather than random chance.
-
Findings: The I2 values indicated moderate to high heterogeneity for several key endpoints, including all-cause mortality in secondary prevention trials (I2=82%) and myocardial infarction in both all trials (I2=82% for ARR) and secondary prevention trials (I2=89% for ARR).
-
Impact: An I2 of over 75% indicates substantial heterogeneity. The authors correctly state that when such significant heterogeneity exists, pooling the results in a meta-analysis may be “ill-advised,” and the findings “may be unreliable.”
Failure to Link LDL-C Reduction to Benefit
A primary goal of the study was to see if larger reductions in LDL-C were associated with larger clinical benefits. The meta-regression analysis, which was designed to test this association, was inconclusive. It failed to establish a consistent or reliable association between the magnitude of LDL-C reduction and the treatment effect on all-cause mortality, MI, or stroke. This challenges the fundamental premise that the clinical benefit of statins is directly mediated by the degree to which they lower LDL-C levels.
Risk of Bias in Included Studies
While the overall risk of bias in the included trials was judged to be low, several important issues were flagged:
-
Industry Funding: All 21 of the included trials were funded, either in part or wholly, by the pharmaceutical industry.
-
Early Termination: Four of the included trials were terminated early, which may be a source of bias, often leading to an overestimation of the treatment effect.
Reporting Quality Assessment (PRISMA)
The review’s reporting quality adheres to the PRISMA statement. The authors provided a flow diagram illustrating the study selection process in the supplement and adequately described their search strategy, meeting key criteria for transparency and reproducibility.
Research Objective
Using the PICO framework:
-
Population: Adults (>18 years) in primary and secondary prevention settings.
-
Intervention: Statin therapy.
-
Comparison: Placebo or usual care.
-
Outcomes: All-cause mortality (primary), myocardial infarction, and stroke (secondary).
The study’s objective was to assess the association between the absolute reduction in LDL-C from statin therapy and the absolute and relative risk reductions in all-cause mortality, MI, and stroke.
Study Design
This is a systematic review and meta-analysis of large, randomized clinical trials. The authors searched the PubMed and Embase databases for RCTs with a planned duration of at least 2 years and more than 1000 participants.
Setting and Participants
The analysis included 21 randomized controlled trials. For the primary outcome of all-cause mortality, data were pooled from 19 trials, encompassing a total of 132,763 participants (66,366 in statin groups and 66,397 in control groups).
Bibliographic Data
-
Title: Evaluating the Association Between Low-Density Lipoprotein Cholesterol Reduction and Relative and Absolute Effects of Statin Treatment: A Systematic Review and Meta-analysis
-
Authors: Byrne P, Demasi M, Jones M, Smith SM, O’Brien KK, DuBroff R.
-
Journal: JAMA Internal Medicine
-
Year: 2022
-
DOI: 10.1001/jamainternmed.2022.0134
Mandatory Disclaimer: This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
Full text PubMed Central