Comment:
I am in general not a fan of intermittent fasting as my experience is it puts the body in a state of stress, which may give short term gains, but longer term negative outcomes. This is a study showing that skipping breakfast increases metabolic syndrome, including blood sugar, blood pressure, blood lipids and central adiposity.
Clinical Bottom Line:
This meta-analysis suggests a significant association between skipping breakfast and an increased risk of Metabolic Syndrome (MetS). However, this conclusion is based on low-certainty evidence derived exclusively from observational studies, which can identify associations but cannot prove causation. The findings are further weakened by substantial statistical heterogeneity across the included studies for several key outcomes, indicating that the magnitude of risk was inconsistent. Therefore, while skipping breakfast may be a marker for increased metabolic risk, it cannot be definitively named as the cause based on this review.
Results
Summary of Results:
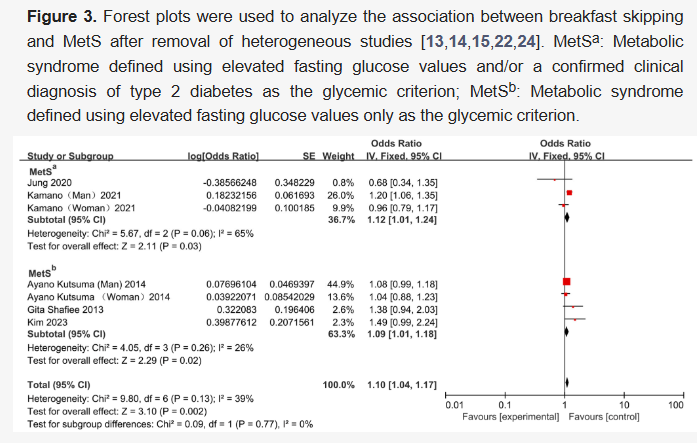
The pooled analysis found that individuals who skipped breakfast had 10% higher odds of having Metabolic Syndrome after a sensitivity analysis was performed to remove a major source of heterogeneity (Pooled Odds Ratio [OR] = 1.10, 95% Confidence Interval [CI] 1.04–1.17). An odds ratio of 1.10 means the odds of having MetS were 1.1 times higher in the breakfast-skipping group compared to those who ate breakfast.
Skipping breakfast was also associated with increased odds of its individual components:
-
Hyperglycemia: OR 1.26 (95% CI 1.16–1.37) (result after sensitivity analysis)
-
Hypertension: OR 1.21 (95% CI 1.10–1.32) (result after sensitivity analysis)
-
Abdominal Obesity: OR 1.17 (95% CI 1.01–1.34)
-
Hyperlipidemia: OR 1.13 (95% CI 1.04–1.23)
Assertive Critical Appraisal
Certainty of Evidence (GRADE Framework):
The authors did not formally use the GRADE framework. As an appraiser, I would rate the certainty of this evidence as ‘Low’. By design, systematic reviews of observational studies start with ‘Low’ certainty because they are at high risk of bias. The primary limitation, which the authors acknowledge, is the potential for unmeasured confounding variables. For example, skipping breakfast may simply be a marker for other unhealthy lifestyle behaviors (e.g., poor overall diet quality, lack of exercise, or circadian rhythm disruption) that are the true drivers of Metabolic Syndrome.
Heterogeneity:
The authors reported significant heterogeneity for the primary outcome of MetS before sensitivity analysis (I2 = 52%). The I2 statistic represents the percentage of variation across studies due to real differences rather than just chance. Even more substantial heterogeneity was found in the initial analyses for hypertension (I2 = 79%) and hyperglycemia (I2 = 73%). An I2 this high indicates substantial inconsistency in the results of the included studies, which weakens the confidence in the pooled average risk. The authors performed sensitivity analyses by removing specific studies to achieve lower heterogeneity, which suggests the overall finding is sensitive to the inclusion of certain studies.
Publication Bias:
The authors state that the funnel plot technique was used to analyze for publication bias. However, they do not report the specific results of this analysis (e.g., visual interpretation or statistical test results) in the main text, which is an omission.
Risk of Bias in Included Studies:
The review used the Newcastle-Ottawa Scale (NOS) to assess the quality of the included observational studies. All nine included studies had scores greater than 6, indicating their quality was “medium or above”. Despite this, the most critical methodological challenge in this body of evidence remains the high risk of residual confounding, which is an inherent limitation of observational study designs.
Reporting Quality Assessment (PRISMA):
The review states it was conducted in accordance with PRISMA 2020 guidelines. It does include a PRISMA flow diagram (Figure 1), which transparently shows the study selection process (9 studies included from 46,055 identified records). The authors also describe their search strategy and the databases used.
Research Objective
The review’s objective, based on the PICO framework, was to investigate the association between skipping breakfast (Exposure) and the prevalence/incidence of MetS and its components (Outcomes) among the general population (Population), compared with individuals who regularly consume breakfast (Comparison).
Study Design
This is a systematic review and meta-analysis of observational studies. The authors systematically searched PubMed, Embase, Cochrane Library, and Web of Science databases from their inception until May 2025. The review included cross-sectional and cohort studies.
Setting and Participants
The analysis included a total of 9 observational studies (eight cross-sectional and one cohort) involving 118,385 participants. The studies were conducted in various countries, including Korea, Japan, the USA, Iran, and Brazil.
Bibliographic Data
-
Title: Association of Skipping Breakfast with Metabolic Syndrome and Its Components: A Systematic Review and Meta-Analysis of Observational Studies
-
Authors: Yang, B.; Lian, L.; Xing, K.; Cen, Y.; Zhao, Y.; Zhang, Y.
-
Journal: Nutrients
-
Year: 2025
-
DOI: https://doi.org/10.3390/nu17193155
This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Summary:
Original Article:
Open Access This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).