Comment:
Although this doesn’t negate the potential of increased risk of atrial fibrillation seen in other studies, a lower rate of death seems more important.
Summary:
Clinical Bottom Line
This large cohort study shows a modest association between habitual fish oil use and a lower risk of all-cause mortality. However, it is not possible to conclude that fish oil causes this benefit. The results are highly susceptible to unmeasured confounding variables, particularly the “healthy user effect,” where individuals who choose to take supplements may also engage in other healthy behaviors not fully captured in the analysis.
Results in Context
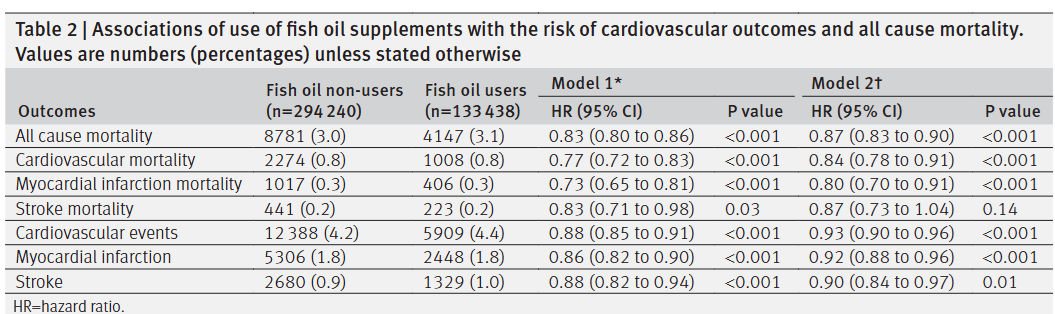
Main Results After adjusting for a wide range of demographic, lifestyle, and health-related factors, habitual users of fish oil supplements had a 13% lower rate of death from any cause compared to non-users over a median follow-up of 9.0 years.
-
Adjusted Hazard Ratio (HR) for All-Cause Mortality: 0.87 (95% Confidence Interval 0.83 to 0.90).
-
Unadjusted HR (for age and sex): 0.83 (95% CI 0.80 to 0.86).
Definitions The primary statistic used is the Hazard Ratio (HR). An HR of 0.87 means that at any given point during the study, an individual in the fish oil user group had a 13% lower likelihood of dying compared to someone in the non-user group, after accounting for the measured confounders.
Participants The analysis included 427,678 individuals from the UK Biobank, of whom 133,438 (31.2%) reported regularly taking fish oil supplements at the start of the study.
Assertive Critical Appraisal
Limitations & Bias (STROBE Framework) The primary weakness of this study is the inherent risk of confounding, which is common to all observational nutritional research.
-
Healthy User Bias: Individuals who take supplements are often more health-conscious in general. While the authors commendably adjusted for many lifestyle factors (e.g., diet, physical activity, smoking), it is nearly impossible to eliminate the possibility that the observed benefit is due to other unmeasured healthy habits rather than the fish oil itself.
-
Crude Exposure Measurement: The study only asked participants if they “regularly take” fish oil supplements (a simple yes/no answer). It did not collect crucial information on the dose, duration, or specific formulation of the supplements. This is a major limitation, as it prevents any analysis of a dose-response relationship, which would strengthen a causal argument.
-
Reverse Causality: It is possible that individuals with developing health problems might stop taking supplements. However, the authors appropriately addressed this by performing a sensitivity analysis that excluded anyone who died within the first two years of follow-up, and the results did not change substantially, which strengthens the findings.
Reporting Quality Assessment (STROBE) The authors clearly described their extensive efforts to address potential sources of confounding by adjusting for a wide range of variables in their statistical models. This detailed reporting meets a key quality standard for observational research.
Applicability The study’s population of middle-aged and older adults from the UK is broadly applicable to patients in general clinical practice in other developed countries. The exposure—over-the-counter fish oil supplements—is common and relevant.
Research Objective
To evaluate the associations of habitual fish oil supplementation with the risk of all-cause mortality, cardiovascular disease (CVD) mortality, and incident CVD events in a large prospective cohort.
Study Design
This was a population-based, prospective cohort study using data from the UK Biobank.
Setting and Participants
The study included 427,678 men and women aged 40 to 69 who were recruited between 2006 and 2010 from 22 assessment centers across the UK. Participants were free of cardiovascular disease and cancer at baseline and were followed up until 2018.
Bibliographic Data
-
Title: Associations of habitual fish oil supplementation with cardiovascular outcomes and all cause mortality: evidence from a large population based cohort study
-
Authors: Zhi-Hao Li, Wen-Fang Zhong, Simin Liu, et al.
-
Journal: The BMJ
-
Year: 2020
This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
Full text pdf: hyperlink here
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.